Patient Record
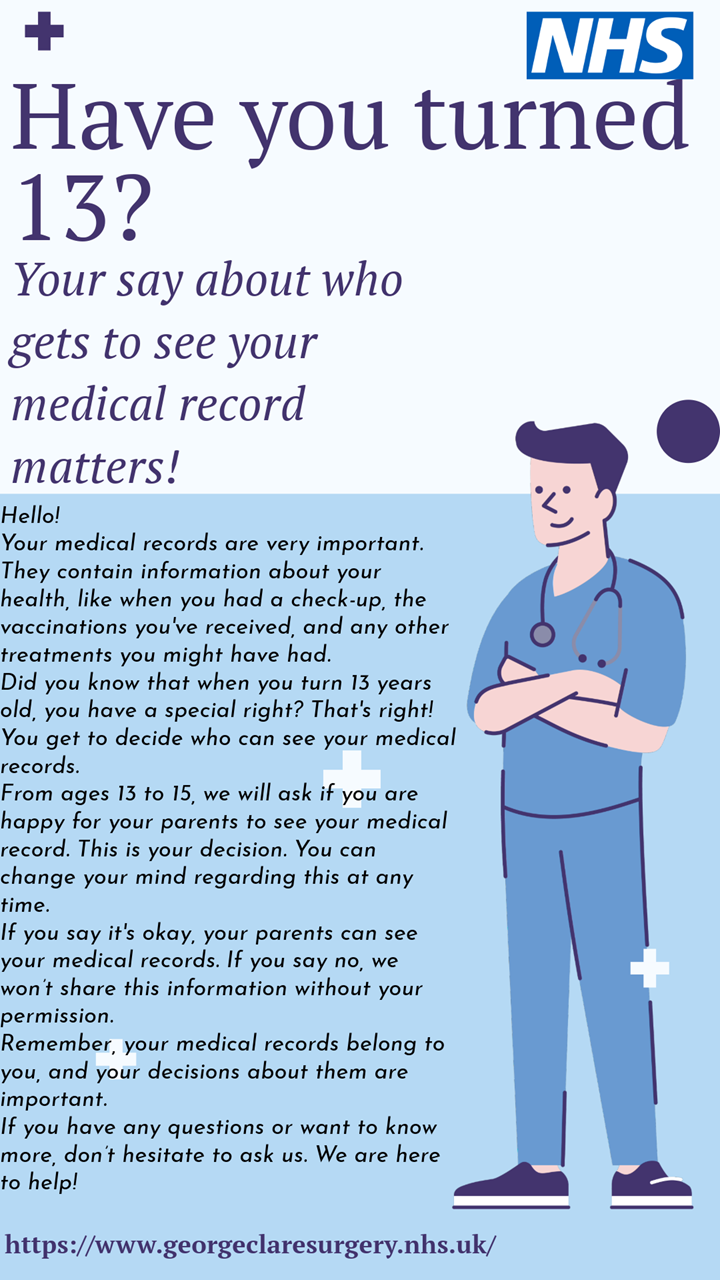
Prospective Medical Record Access from 31/10/2023
As your GP practice, we have been asked to provide you with access to your full medical record via the NHS app (and NHS website) if you have a suitable NHS login, from 31 October 2023.
As a practice we have decided to ask your permission first, as this gives us a chance to check your understanding and be sure access to your data is safe for you.
We are aware that not everyone will want access to their full record on the internet at this time, and some patients may have concerns about their personal medical records being made available on their smartphones or online, especially if other people have access to their devices.
You can change your mind at any time by contacting the practice.
If you do NOT want access, please reply NO to the sms sent to you or inform Reception
For further information on prospective record access please visit https://www.nhs.uk/nhs-app/
Added 20/10/23
Sharing Your Medical Record
Increasingly, patient medical data is shared e.g. between GP surgeries and District Nursing, in order to give clinicians access to the most up to date information when attending patients.
The systems we operate require that any sharing of medical information is consented to by patients beforehand. Patients must consent to sharing of the data held by a health provider out to other health providers and must also consent to which of the other providers can access their data.
e.g. it may be necessary to share data held in GP practices with district nurses but the local podiatry department would not need to see it to undertake their work. In this case, patients would allow the surgery to share their data, they would allow the district nurses to access it but they would not allow access by the podiatry department. In this way access to patient data is under patients' control and can be shared on a 'need to know' basis.
Summary Care Record
There is a new Central NHS Computer System called the Summary Care Record (SCR). The Summary Care Record is meant to help emergency doctors and nurses help you when you contact them when the surgery is closed. Initially, it will contain just your medications and allergies.
Later on as the central NHS computer system develops, (known as the ‘Summary Care Record’ – SCR), other staff who work in the NHS will be able to access it along with information from hospitals, out of hours services, and specialists letters that may be added as well.
Your information will be extracted from practices such as ours and held on central NHS databases.
As with all new systems there are pros and cons to think about. When you speak to an emergency doctor you might overlook something that is important and if they have access to your medical record it might avoid mistakes or problems, although even then, you should be asked to give your consent each time a member of NHS Staff wishes to access your record, unless you are medically unable to do so.
On the other hand, you may have strong views about sharing your personal information and wish to keep your information at the level of this practice. Connecting for Health (CfH), the government agency responsible for the Summary Care Record have agreed with doctors’ leaders that new patients registering with this practice should be able to decide whether or not their information is uploaded to the Central NHS Computer System.
For existing patients it is different in that it is assumed that you want your record uploaded to the Central NHS Computer System unless you actively opt out.
Click here to download the consent form
Page created: 04 December 2019